

 Back to Suggested Publications
Back to Suggested Publications
This week WAidid suggests the article A Placebo-Controlled Trial of Antibiotics for Smaller Skin Abscesses, recently published on the NEJM.
SUMMARY
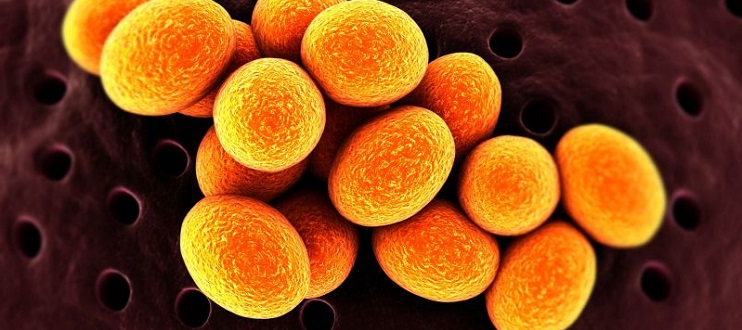
Uncomplicated skin abscesses are common. Staphylococcus aureus (S. aureus), including methicillin-resistant S. aureus (MRSA) strains, causes most of skin infections. Clindamycin and trimethoprim–sulfamethoxazole (TMP-SMX) are recommended for outpatient treatment of these infections, but data on their safety and efficacy are limited.
The authors report the results of their multicenter, prospective, randomized, double-blind, placebo-controlled clinical trial. Between May 2009 and January 2015, 786 outpatients participants with a single skin abscess, 5 cm in diameter or smaller, were randomly assigned to receive, in a 1.1:1 ratio, oral clindamycin (266 patients), TMP-SMX (263 patients) or placebo (257 patients) for 10 days, in addition to incision and drainage. 281 (35.8%) of the subjects enrolled were children. A total of 343 participants were fully adherent to the study regimen.
S. aureus was isolated in 527 (67.0%), MRSA in 388 (49.4%), coagulase-negative staphylococci in 104 (13.2%), streptococcus species in 54 (6.9%), and other organisms in 118 (15.0%).
The rates of clinical cure were 83.1% in the clindamycin group, 81.7% in the TMP-SMX group, both significantly higher than that of placebo group (P< 0.001), with no differences between the two treatment groups. This beneficial effect was restricted to participants with S. aureus infection.
Children had a significantly higher cure rate with clindamycin than with TMP-SMX or placebo, greater than that seen among adults.
Clindamycin may be more effective than TMP-SMX in preventing recurrences or new infections, after completion of therapy, particularly in children: the difference in the rates of interval or recurrent infections, between the TMP-SMX and clindamycin groups, was significant (P = 0.03), but the difference, between the placebo and clindamycin groups and the difference between the placebo and TMP-SMX groups, were not significant.
The rate of treatment-associated adverse events was higher in the clindamycin group than in the TMP-SMX group or in the placebo group. The most common adverse events were diarrhea and nausea.
The authors conclude that short-term outcomes, among patients with uncomplicated cutaneous abscesses, particularly those caused by S. aureus, are improved by antibiotic treatment with either clindamycin or TMP-SMX in addition to abscess incision and drainage, but that this benefit must be weighed against the known side-effect profile of these antimicrobials.
AUTHORS: Robert S. Daum, Loren G. Miller, Lilly Immergluck, Stephanie Fritz, C. Buddy Creech, David Young, Neha Kumar, Michele Downing, Stephanie Pettibone, Rebecca Hoagland, Samantha J. Eells, Mary G. Boyle, Trisha Chan Parker, and Henry F. Chambers
Click here to go to the article.