

 Back to Suggested Publications
Back to Suggested Publications
This week WAidid suggests the article Autism Spectrum Disorders and the Gut Microbiota, recently published on "Nutrients"
Autism spectrum disorder (ASD) is a complex group of developmental disorders characterized by impaired social interactions and communication together with repetitive and restrictive behaviours, which represents a serious public health problem. The authors reviewed literature on this topic.
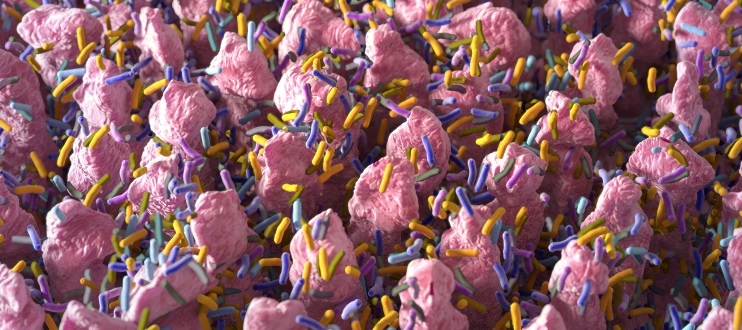
Various factors have been associated with the development of ASD, including both genetic and environmental factors: environmental factors are now believed to play a much more important role than previously assumed. Even if the exact etiopathogenesis of ASD is poorly understood, in recent decades, research has pointed to the interaction between the gut microbiota and the brain in patients with autism or other neuropsychiatric diseases. A considerable number of subjects with ASDs have significant gastrointestinal dysfunctions; their gastrointestinal (GI) symptoms seem to correlate strongly with the severity of their ASD.
The microbiota plays a contributory role in many infections, immune-mediated disorders, rheumatologic diseases and disorders of the nervous system. In recent years, several studies have shown significant changes in the composition of the gut microbiota in children with ASD and have suggested that GI symptoms in ASD may be a manifestation of the underlying inflammatory process. Indeed, the gut microbiota and the related metabolites play a crucial role in the so-called “gut-brain axis”.
There is evidence that autistic individuals have maldigestion and malabsorption problems; dysbiosis of bacterial species and yeasts have been reported in ASD subjects. Although many studies have been published on dysbiosis in the gut microbiota of individuals with ASD, there is still little consensus on the exact composition of the gut microbiome that is specific to individuals with ASDs.
Individuals with ASD seem to have decreased digestive enzyme activity and impaired protein digestion that, together with increased gut permeability, could be responsible for the elevated levels of urinary dietary peptides, altered plasma amino acid profiles and high levels of faecal putrefactive metabolites reported in children with ASD.
Currently, no definitive or effective therapies for ASD exist. The approved and recommended treatments for ASD essentially include rehabilitation, educational therapy and psycho-pharmacological approaches.
Dietary interventions in children with ASD are very popular, but could be potentially harmful. Probiotic administration could represent a potential better alternative to restrictive dietary interventions because, in addition to general safety and tolerance, probiotics can heal the intestinal mucosa, protect the epithelial barrier through the production of mucin and fortifying tight junctions, increase the production of digestive enzymes and antioxidants, and modulate the immune response. Faecal microbiota transplant (FMT) and microbiota transfer therapy (MTT) have recently attracted the interest of researchers due to their possible effect to alleviate GI and neurobehavioural symptoms, by rebalancing the physiological intestinal microbiota.
To learn more, go to the article https://www.ncbi.nlm.nih.gov/pubmed/30823414